Dealing with an enlarged prostate can be challenging, but there are paths to relief. This article explores prostate artery embolization (PAE), a minimally invasive procedure for benign prostatic hyperplasia (BPH). We’ll cover the PAE procedure, recovery, benefits, and risks, with insights from a board-certified urologist, Dr. Mistry, and Donna Lee, Director of Business Development at Urology Specialists of Austin.
Understanding BPH and the Role of PAE
Benign prostatic hyperplasia (BPH) occurs when the prostate gland enlarges, often squeezing the urethra and causing uncomfortable urinary tract symptoms. The likelihood of developing BPH increases with age, affecting over 80 percent of men.
Medications can manage BPH, but they might not fully relieve everyone and can cause side effects like erectile dysfunction. PAE offers a solution for men seeking alternatives to traditional surgery.
Exploring PAE: A Minimally Invasive Procedure
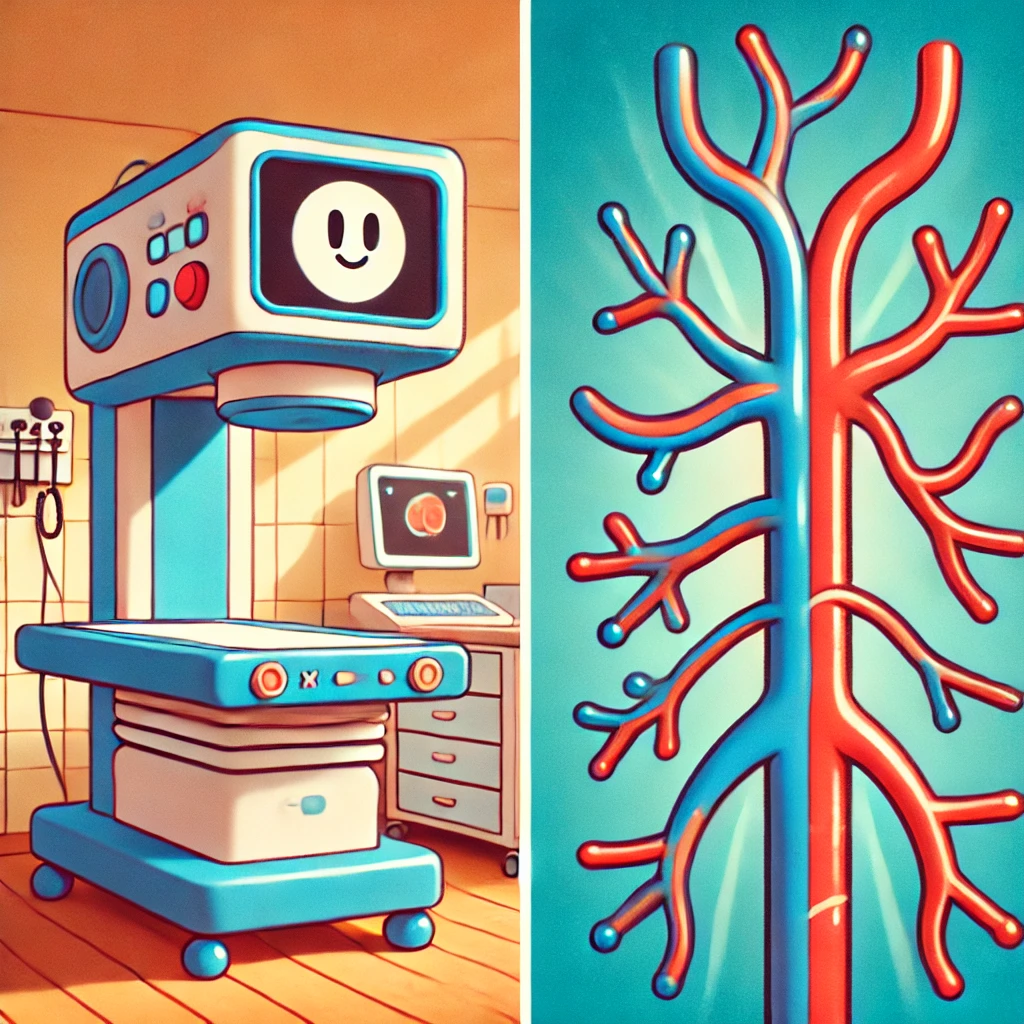
Prostate artery embolization (PAE) is a different approach to treating BPH. This image-guided procedure blocks blood flow to the prostate gland, shrinking it. Let’s explore it further.
How Does PAE Work?
An interventional radiologist inserts a small catheter into an artery, usually in the wrist or groin. Guided by imaging, the catheter reaches the prostate arteries.
Microscopic beads are injected to obstruct blood flow, causing the prostate to shrink. This minimizes disruptions compared to surgery. PAE may be an option for those not suited for or interested in traditional BPH surgery.
An exam with an interventional radiologist can confirm PAE candidacy, assessing urinary symptom frequency and daily life impact. This is often one of the first steps in improving urinary tract symptoms.
What is the Recovery Time for PAE?
PAE recovery typically involves minimal downtime, according to Northwestern Medicine. Patients go home the same day and resume normal activities shortly after. Pain relievers and antibiotics can alleviate discomfort.
Weighing the Pros and Cons of PAE
Every treatment has advantages and disadvantages. The best choice depends on individual circumstances. Some individuals may experience “post-PAE syndrome” (nausea, pelvic pain, changes in urination) after the procedure.
Benefits of PAE
- Minimally invasive: Smaller incisions, less scarring, and faster healing.
- Reduced risk of complications: Lower chances of sexual or urinary dysfunction than traditional surgeries. Northwestern Medicine reports 80%-90% urinary symptom improvement in many PAE patients. Some studies suggest PAE may offer relief comparable to TURP with potentially fewer side effects. This information can be useful for those experiencing urinary incontinence.
- Preserved sexual function: Often avoids sexual side effects linked with other BPH surgeries, although factors like embolization extent and individual variability matter. One-sided embolization may be used, sometimes allowing medications like Tadalafil or Sildenafil to help maintain erectile function. Other sexual function issues may not be related to PAE.
- Quick recovery: Most return to daily routines quickly.
Risks and Potential Complications of PAE
- Post-embolization syndrome: Some experience mild side effects like pelvic discomfort, fever, and urinary tract symptoms. NSAIDs can often help with these symptoms caused by the prostate.
- Not suitable for all: Blockages may require surgical intervention.
- Long-term effectiveness: Results can vary. PAE engineers are working on solutions for this, although long term research still needs to be completed to see what kind of success can be seen from PAE.
Making an Informed Decision: Is PAE Right for You?
Finding relief from prostate issues starts with talking to a qualified physician. Openly discussing concerns and medical history helps doctors create management plans. Dr. Mistry, specializing in men’s health and low testosterone, has provided urologic care for years with Donna Lee.
Second opinions are helpful. Medical record reviews or telehealth appointments can offer guidance. Independent sources can provide diverse PAE perspectives. This broadens the discussion on PAE’s role in treating urinary tract symptoms. For more personalized assistance, consult with PAE engineers about the procedure performed in more detail.
Conclusion
Navigating BPH treatments requires understanding individual conditions, pros, cons, and long-term expectations. PAE is a less disruptive way to improve symptoms. It is a growing treatment area for BPH, but it doesn’t replace all established therapies.
Consulting physicians with PAE experience, exploring treatment approaches like those at Urology Specialists of Austin (512-238-0762), and reviewing resources like the Inova Health Library or Inova Newsroom are essential when deciding if PAE is a good option.
Discuss your options with your urologist. Talking openly allows them to help you make healthcare choices and create wellness plans. Being involved in healthcare decisions is empowering, as they hold significant impact.